Why I started this website
In recent years, I’ve noticed a disconnect between the scientific advancements in our understanding of how the gut and the brain work, including the implications of the interactions between the mind and body, and the awareness of these advances among practitioners and the public. There is clearly a need for the dissemination of research findings. The challenge for this is that “translating” and interpreting science accurately requires deep knowledge of physiology, immunology, neuroscience, and behavior. For these reasons, I’m writing educational “blog posts” for this website, to (hopefully) make this information available to anyone, regardless of their background.
Growing Up
From time to time when I was a little girl, grown-ups would ask me “what do you want to be when you grow up?” I always said I didn’t know, but that wasn’t true. I knew I wanted to be a scientist when I grew up. I loved everything about the natural world and I devoured books and encyclopedias about topics in evolution (horses and dinosaurs!), geology, astronomy, biology, and later, psychology. I imagined a romanticized world of white-coated discovery.
I said I didn’t know what I wanted to be because everyone in the 1960s knew that little girls could not grow up to be scientists. As my 7th-grade science teacher said- “everyone knows boys are smarter in science than girls”. But fortunately for me, things changed in the 1970s and 1980s, and it became possible for girls like me to grow up to be scientists.

Why I chose this field
Physiological Psychology studies how the nervous system and the rest of the body collaborate to regulate bodily functions (i.e. digestion and blood pressure) and how what’s happening in the body influences brain functions, including thinking and behavior. The goals are to understand the mechanisms of these interactions and how they enable us to maintain health and respond to challenges, both mental and physical. It seemed to me that this was something I could spend my life studying and staying passionate about. And I have. My life as a scientist has been exciting and emotionally rewarding.
I first became interested in psychology as a teenager (my mother had a subscription to Psychology Today). When I went to college at the University of Washington in Seattle, I assumed I would go into Clinical Psychology. But while taking classes in Physiological Psychology, I fell in love with the brain. Working in the laboratories of Dr. Ilene Bernstein and Dr. Steve Woods started me on a “brain-gut odyssey” exploring the relationships between food, the gut, and how what is happening in the gut influences behavior, motivation, and mood.
My PhD
I left Washington to do graduate work with Dr. Don Novin at UCLA. where I studied gut and liver interactions with the brain. Don taught me the importance of taking a bigger, more holistic view of the regulation of physiology and behavior, and the importance of bottom-up “gut factors”.
During my time at UCLA I realized that if I wanted to understand the mechanisms of how the gut and liver influence health and behavior, I needed to “get under the hood”. That is- I needed to understand the physical connections between the abdominal viscera and the brain. Fortunately for me, I had the opportunity to train in anatomy with Dr. Catia Sternini and Dr.Nick Brecha, at the Center for Ulcer Research and Education (CURE) which is now the Digestive Diseases Research Center at UCLA. At CURE, I gained an appreciation for gut structure and function and how the “gut-brain” (enteric nervous system) coordinates the complex processes of digestion and metabolic regulation. I am incredibly grateful for the advice and mentorship, and for how Katia and Nick emphasized rigorous scientific design, methodology, and scholarship. Nick once noted that “the kind of answers you get depend on the questions you ask”. I still think about that.
Post-Doctorate
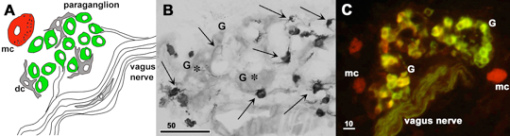
After receiving my Ph.D. in Psychology (Physiological Psychology) from UCLA, I joined the laboratory of Dr. Tom Finger at the University of Colorado Health Science Center for post-doctoral adventures in the comparative anatomy of the autonomic nervous system. This work enabled me to gain a further, more comprehensive understanding of the gut and how it communicates with the brain.
I landed in my current field, Psychoneuroimmunology, as a result of my collaboration with Linda Watkins and Steve Maier at CU Boulder, in which we showed that sensory vagus nerves serve as a major pathway by which the immune system and brain communicate. This vagal pathway provides a mechanism by which gut problems can lead to symptoms such as depression, anxiety, fatigue, or “cognitive fuzziness”. Research by other groups showed that the vagal motor nerve can reduce inflammation, which may be a mechanism by which mind-body modalities such as meditation, massage, or yoga that activate the vagus nerve exert their beneficial effects.
I love the vagus nerve.
Further Research
In 2000, I relocated to the University of Virginia (UVA), where I continued basic science studies of vagal-related pathways and their effects on inflammation or “sickness” symptoms. Highlights include the demonstration that inflammation inhibits brain systems involved with arousal and motivation (including dopamine and histamine systems) and this likely contributes to the mood and behavior problems common in conditions involving inflammation. In a collaboration with Dr. Mark Lyte, we showed that administration of a load of gram-negative bacteria to the gut activates vagal sensory neurons and brain networks that are associated with anxiety and stress. These studies were among the very first to show that gut bacteria can influence the brain and behavior. After eight years, I relocated to the Center for the Study of Complementary and Alternative Therapies (CSCAT) at the School of Nursing (UVA), which was directed by Dr. Ann Taylor. While at CSCAT, I gained an appreciation of the joys and challenges of research with humans. A key finding from my work there was that pain symptoms in people with fibromyalgia are related to an interaction of stress (including sleep problems) with the programming of immune cells. That is: compared to controls, stress seems to lead to more pro-inflammatory type immune cells in the blood of people with fibromyalgia. Inflammation causes and enhances pain, so these studies provide a mechanistic link between fibromyalgia symptoms and stress.
Exploring Mind-Body Modalities
In recent years, basic and clinical studies have continued to show powerful anti-inflammatory effects of the vagus nerve. Traditional approaches for stimulating the vagus have been invasive and potentially expensive, limiting its availability to many people who are suffering from inflammation-related conditions but are not able to afford the therapy. It seems to me that mind-body modalities that activate the vagus nerve can be cost-effective ways to help the body heal. To this end, I trained with Siggy Bonnevie in Restorative Yoga, and with Tussi Kluge and Leslie Blackhall in Mindfulness-Based Stress Reduction. As these are relaxation-based modalities, they could be helpful for stress and inflammation in people who have mobility problems or are in the hospital. Although I was not able to do studies using these modalities, as I had hoped to do, recent studies have supported and reinforced the idea that they can be powerful therapeutic approaches. I can attest to that from my personal experience. I suffered for several years with musculoskeletal pain that I believed was going to be permanent, but after adopting an “interoceptive meditation” (something of a combination of the two modalities) practice, my pain has essentially gone into a long-lasting remission.
In summary
Over the years I have continued to address what I think of as the biological bases for mind-body interactions and talk about my work all over the United States and in Europe (see the Curriculum Vitae tab for details). I have had the opportunity to teach thousands of students, on topics including Psychology of Perception, Neuroscience, Mind-Body Interactions, Stress, Emotions, and the Brain, and Developmental Psychology. As a speaker with the Institute for Brain Potential, I have traveled around the United States providing educational seminars on topics related to gut health and gut-brain interactions, diet and brain health, and implications of inflammation diet and “how we feel”.
For anyone interested – I’m happy to speak to public/patient/practitioner groups on topics related to gut problems, stress and resilience, mood, inflammation, healthy aging, and mindful eating.

Selected References
Bernstein, I.L., & Goehler, L.E. Vagotomy produces learned food aversions in the rat. Behavioral Neuroscience, 97:585-594, 1983.
Bernstein, I.L., Treneer, C.M., Goehler, L.E., & Murochick, E. Tumor growth in rats: conditioned suppression of food intake and preference. Behavioral Neuroscience, 99:818-830, 1985
Gaykema, R.P.A., Goehler, L.E., & Lyte, M. Brain response to cecal infection with Camplyobacter jejuni: analysis with Fos immunohistochemistry. Brain, Behavior, and Immunity, 18:238-245, 2004. PMID: 15050651
Goehler, L.E., Sternini, C., & Brecha, N.C. Calcitonin gene-related peptide immunoreactivity in the biliary pathway and liver of the guinea pig: distribution and colocalization with substance P. Cell and Tissue Research, 253:145-150, 1988.
Goehler, L.E., & Sternini, C. Neuropeptide Y immunoreactivity in the mammalian liver: pattern of innervation and coexistence with tyrosine hydroxylase immunoreactivity. Cell and Tissue Research, 265:287-295, 1991.
Goehler, L.E., & Finger, T.E. Functional organization of vagal reflex systems in the brainstem of the goldfish Carassius auratus. Journal of Comparative Neurology, 319:463-478, 1992.
Goehler, L.E., Gaykema, R.P.A., Hammack, S.E., Maier, S.F. & Watkins, L.R. Interleukin-1 induces c-Fos immunoreactivity in primary afferent neurons of the vagus nerve. Brain Research, 804:306-310, 1998.
Goehler, L.E., Gaykema, R.P.A., Nguyen, K.T., J.L. Lee, Tilders, F.J.H., Maier, S.F., & Watkins, L.R. Interleukin-1β in immune cells of the abdominal vagus nerve: an immune to nervous system link? Journal of Neuroscience, 17:2799-2806, 1999.
Goehler, L.E., Gaykema, R.P.A., Anderson, K., Hansen, M.K., Maier, S. F., & Watkins, L.R. Vagal immune-to brain communication: a visceral chemoreceptive pathway. Autonomic Neuroscience, 85:49-59, 2000
Goehler, L.E., Gaykema, R.P.A., Opitz, N., Reddaway, R., Badr, N.A., & Lyte, M. Activation in vagal afferents and central autonomic pathways: early responses to intestinal infection with Campylobacter jejuni. Brain, Behavior, and Immunity, 19:334-344. 2005. PMID: 15944073
Goehler, L.E., Erisir, A., & Gaykema, R.P.A. Neural-immune interface in the area postema. Neuroscience, 140:1415-1434, 2006. PMID: 16650942
Goehler, L.E., Lyte, M., & Gaykema, R.P.A. Invited Minireview: Infection-induced viscerosensory signals from the gut enhance anxiety: implications for psychoneuroimmunology. Brain Behavior and Immunity; 6:721-6, 2007. PMID: 17428636
Jallo N., Bourguignon, C., Taylor, A.G., Ruiz, J., & Goehler, L. The biobehavioral effects of relaxation guided imagery on maternal stress. Advances in Mind Body Medicine, 24:12-22, 2009. PMID: 20671330
Kinser, P., Goehler, L.E., & Taylor, A.G. How might yoga help depression? A neurobiological perspective. EXPLORE: The Journal of Science and Healing, 8(2):118-126, 2012.
Maes, M., Berk, M., Goehler, L., Song, C., Anderson, G., Galecki, P., & Leonard, B. Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Medicine, 10:66, 2012. doi:10.1186/1741-7015-10-66
Marvel, F.A., Chen, C.-C., Badr, N.A., Gaykema, R.P.A., & Goehler, L.E. Reversible inactivation of the dorsal vagal complex blocks lipopolysaccharide-induced social withdrawal and c-Fos expression in central autonomic nuclei. Brain, Behavior, and Immunity, 18:123-143, 2004. PMID: 14759590
Park, S,-M., Gaykema, R.P.A., & Goehler, L.E. How does immune challenge inhibit ingestion of palatable food? Systemic lipopolysaccharide modulates key nodal points of feeding neurocircuitry. Brain, Behavior and Immunity, 22:1160-172, 2008. PMID: 18562160
Taylor, A.G., Goehler, L.E., Galper, D.I., Innes, K.E., & Bourguignon, C. Top-down and bottom-up mechanisms in mind-body medicine: development of an integrative framework for psychophysiological research. EXPLORE: The Journal of Science and Healing, 6:29-41, 2010. PMID: 20129310
Taylor A.G,. Fischer-White T.G., Anderson J.G., Adelstein K.E., Murugesan M., Lewis J.E., Scott M.M., Gaykema R.P., Goehler, L.E. Stress, Inflammation and Pain: A Potential Role for Monocytes in Fibromyalgia-related Symptom Severity. Stress and Health, 32:503-513, 2016
Watkins, L.R., Wiertelak, E.P., Goehler, L., Mooney-Heiberger, K., Martinez, J., Furness, L., Smith, K.P., & Maier, S.F. Neurocircuitry of illness-induced hyperalgesia. Brain Research, 639:283-299, 1994
Watkins, L.R., Maier, S.F., & Goehler, L.E. Immune activation: The role of proinflammatory cytokines in inflammation: illness responses and pathological pain states. Pain, 63:289-302, 1995